Side Effects - Cancer Pain
What is Pain?
- Pain is whatever you say is painful, happening whenever and wherever you say it does
- There are many different kinds of pain
- It may be an unpleasant feeling/ hurting
- It may feel sharp, dull, burning, numbing, or shooting
- It may not be much of a problem or may be a big problem
- It may last a short time (acute) or a long time (chronic)
- Pain is related to both the area that is hurt and how your brain deals with the signals/ symptoms of pain from this area
- Each person reacts to pain differently (some will experience more pain than others even when the cause of the pain is the same)
- Each person reacts to a specific pain medication/drug different (some will have a lot of pain relief; others will have only a little pain relief with the same type and dose of the pain drug)
Traditional ways of thinking about pain
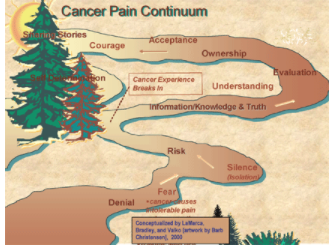
- Pain as a path
- Your path with pain changes as you go through your cancer experience
- As illustrated in Barb Christensens drawing, the path has a lot of twists and turns and personal adjustments as you learn to cope with pain
Jared, insert NACES/CancerPianContinuum,png here please 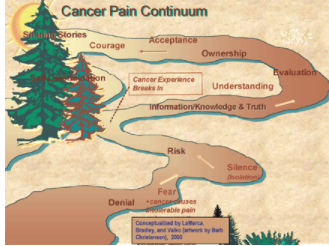
- Pain as part of the Medicine Wheel or Circle of Life
- The physical pain is usually a temporary part of our lives while we go through our cancer experience.
- Most of us can find good ways to deal with pain and get back into balance.
Jared, insert NACES/CancerPain_MW.pgn here please 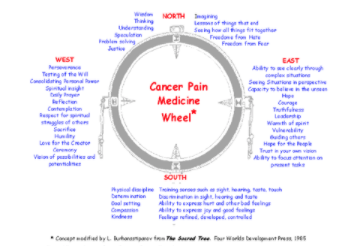
Overall Goal of Pain Relief
- The main goal of pain relief is to decrease the effect of your pain on your comfort, lifestyle, and quality of life
- Methods to treat your pain may not totally get rid of your pain, but should make it so that you can do the things you want to
- If you have pain, it is always important to tell your provider
Managing your pain
- The best method to manage your pain is to prevent it from happening or to treat it early so that it does not become severe
- Cancer pain almost always can be eased if not removed
- Managing your pain is part of your overall cancer treatment
- Satisfactory pain relief
- This is the level of pain that may be noticeable but not bothersome, so you can do what you want and need to do throughout the day (and sleep at night)
- Your pain level should make it easy to sleep, eat and perform other activities
- Medicine: both long lasting and short term
- Heat: compresses and hot pads
- Cold: ice packs
- Massage: to reduce muscle tension and stress
- Traditional Healing: prayers, ceremony
- Herbal Remedies: roots, teas, compresses
- Eastern Practices: acupuncture for example
- Combinations
- Often people get the most relief from a combination of treatments including medicine and hot or cold compresses
- Many people have also benefitted from hypnosis and other mind therapies
Why is pain relief important?
- Pain puts stress on the mind, body and spirit
- Pain interferes with life activities such as sleep, relationships and enjoyment of life
- Pain may interfere with cancer treatment
- Traditional Indian Medicine says that the body should not hurt; pain tells us something is wrong or not in balance
- Helping you understand your pain may help you get the pain relief you need to improve your ability to function and enjoy daily living
How common is cancer pain?
- Surgical pain is common
- 1/3 of people getting chemotherapy have pain
- At least 2/3 of people with advanced cancer have pain
- Those with breast and prostate cancer are most likely to have pain as opposed to those with other types of cancer
- Pain may be the first sign of cancer
- Pain is likely to occur if there is a delay in getting cancer diagnosis and treatment
- American Indians and Alaska Natives frequently deny that they are having any pain (even if pain exists)
- American Indians and Alaska Natives are usually under-treated for pain
Ways to think about pain
- Body Location where the pain is located such as low back pain
- Duration - how long the pain lasts (acute, chronic)
- Cause - what caused the pain such as injury or cancer
- Severity/Intensity - how bad the pain is (0-10 scale)
Pain Threshold
- The time at which something is felt as painful
- Your pain threshold is when you feel something as painful
- It is different for each person (some people feel pain more easily than others)
- Having pain for a long time (chronic pain) does not lead to decreased feelings of pain (just because you have pain for a long time, doesnt mean that you don't feel it or will feel it less)
Pain Tolerance
- Your tolerance is how much pain you can put up with before you want relief from it
- It is different from person to person (some can take much more pain than others)
- A common myth is that if you can put up with a lot of pain then you are able to tolerate even more pain in the future. Having pain or feeling a lot of pain does not help you to better deal with any pain you may have in the future
Drug Tolerance
- After you take your pain medicine for a while, you may need more of it to get the same pain relief (this is called drug tolerance)
- If your disease has not gotten worse, you usually will not need to take more of the medicine to get the same pain relief
- You may have tolerance to the side effects (nausea, sleepiness) of your pain medicine
- Tolerance to side effects is common. It is helpful as you should have fewer problems
- Tolerance also occurs if you are taking traditional medicines such as teas
Physical Dependence
- Physical dependence is NOT addiction
- It is when your body is used to having the narcotic pain medicine because you have been taking it for awhile
- When the narcotic pain drug is stopped suddenly, you have withdrawal symptoms (shaking, aches, sweating)
- The symptoms will be less if the dose of narcotic is slowly lowered once your pain has gotten less or gone away
- It is common with many drugs (if you quickly stop your blood pressure medicine, your blood pressure may go very high, even higher than it was before you started the medicine)
-
Addiction and Substance Dependence
- A psychological dependence (feeling a high when taking the drug); not a physical need (having pain)
- There is no medical need for the drug
- The person has a loss of control, wants or needs the drug even if getting the drug is dangerous or illegal
- Differences between a person which chronic pain and one who is an addict (see table)
| Person with Chronic Pain | Person who is an Addict |
|---|---|
| Takes pain medication when supposed to | Takes pain medicine when desires, even if has no pain |
| When have side effects, usually decreases does of pain medicine | Continues or even increases pain medicines even if has bad side effects |
| Taking pain medicines ease pain and improve QOL | Taking pain medicines may decrease QOL |
| Has concerns about physical problems causing pain | Unaware or denies any problems leading to taking pain medicines |
| Follows directions for taking pain medicines as planned with provider | Doesnt follow directions for taking pain medicine (medicine may not have been ordered by the provider) |
| Often has medicine left over because doesnt take all that is ordered (due to concern about taking too much, not having enough if need it or side effects) | Has no leftover medicines; often runs out before next prescription is due to be filled; often has stories about lost/ stolen medicines |
Rights and Responsibilities of the Patients with Pain
- It is important for you to understand that you have both rights and responsibilities when it comes to pain management
- You need to work with your provider (and your family and friends if you want) to make your concerns about pain and pain management known
- Patient rights related to pain management; I have the right to:
- Have my reports of pain believed and acted on by my providers
- Have my pain controlled, no matter what its cause or how severe it may be
- Expect that my providers will know how to manage my pain or will refer me to someone who does
- Be treated with respect at all times
- When I need medication for pain, I should not be treated like a drug abuser
- Have my cultural beliefs about pain be considered when pain management plans are being made
Patient responsibilities related to pain management; I need to:
- Ask my provider what to expect regarding pain and pain management
- Discuss my pain relief options with my providers
- Work with my providers to develop a pain management plan
- Ask for pain relief when the pain first begins
- As a person with pain I need to:
- Help my providers assess/evaluate my pain
- Tell my providers if my pain is not relieved
- Tell my providers about any worries I have about taking pain medications
Barriers to Cancer Pain Management
- Lack of good cancer pain control policies in IHS / Tribal clinics, due to:
- Myths about cancer patients becoming addicted to pain medications
- Some narcotics having a high street / illegal value (i.e., stolen from the cancer patient and sold to drug abusers in the community)
- Lack of staff in rural or bush regions who can legally prescribe narcotic medications.
- Lack of funding or secure storage facilities for local IHS / Tribal clinics to stock narcotic drugs
- Valuing stoicism - Indians/big boys/girls dont cry
- Having a No pain, no gain philosophy (tough it out)
- Assuming all drugs are bad rather than using drugs in the dose and frequency as prescribed by the provider (Just say no to drugs)
- Being unclear or not understanding about physical dependence, tolerance and addiction
- Barriers: Reluctance to report cancer pain
- Fear having pain means my cancer is getting worse
- Want to be a good patient; my provider is very busy (I didnt want to bother him about my pain)
- Concern I may distract my provider from treating my cancer
- Belief that pain happens to all cancer patients; there is nothing I can do about it
- Barriers: Reluctance to take pain medicines
- Fear of addiction
- Fear my family will view me as an addict
- Worries about side effects
- Concern that there won't be enough medicine for me to take if/when my pain gets really bad if I take some now when the pain isn't really that bad
Keys to Managing your Pain
- The best method to manage your pain is to prevent it from happening or to treat it early so that it does not become severe
- Cancer pain almost always can be eased if not removed
- Managing your pain is part of your overall cancer treatment
- Setting goals for pain relief
- Includes both comfort and function
- The amount of pain relief you want or need may be different for different activities (less amounts for when you have to concentrate and use physical skills for your work, less amounts when you are taking care of your children or grandchildren)
- You and your provider need to decide when pain medicines should be changed (increased or decreased)
- This means you have to tell your provider how you are feeling when you take and do not take the pain medicines (including the side effects you have that may be related to the drugs)
- You need to be honest with your provider and not pretend things are better or worse than what they really are
Satisfactory pain relief
- This is the level of pain that may be noticeable but not bothersome, so you can do what you want and need to do throughout the day (and sleep at night)
- Your pain level should make it easy to sleep, eat and perform other activities
| How pain may feel | |||
|---|---|---|---|
| Achy | Throbbing | Dull | Sharp |
| Stabbing | Squeezing | Pressure | Bloating |
| Cramping | Burning | Shooting | Numb |
| Gnawing | Exhausting | Prickly | Electrical sensation |
Ways to give pain medicine
1. By mouth as a pill or something to suck on (oral) or under the tongue (sublingual) or on the gums
2. Placed on the skin (transdermal)
3. By a suppository placed in the rectum (rectal)
4. By an needle:
- into a muscle (intramuscular, IM)
- under the skin (subcutaneous, SC)
- or through a vein (intravenous, IV)
- by continuous (all the time) infusion (IV) using either a device/pump connected to an IV line)
5. Into the spine (intraspinal, epidural, intrathecal)
- A small needle or small flexible tube is placed into space around the spinal cord area and the pain medicine is injected
- Can be used for short term (2 to 3 days) or long term (weeks to months) pain relief
Way to Manage Cancer Pain
- Medicines for pain management
- Non-narcotics such as Aspirin, Tylenol or Advil
- Narcotics such as Morphine, Dilaudid or Fentanyl
- Additional medicines (called adjuvant because they are given with the pain medicines)
- Steroids such as prednisone (not the same as what athletes may take)
- Antidepressants/mood elevators such as Elavil or Prozac
- Local anesthetics such as Lidocaine
Types of pain medicines based on how often they are given
Short acting drugs
- Last 2-6 hours depending on drug (such as short acting morphine)
- Long acting drugs
- Last 12 to 24 hours or longer (such as long acting morphine which lasts about 12 hours. There is a new oral drug that works for 24 hours and a fentanyl patch works for up to 72 hours)
- Breakthrough medicines (given when pain medicine stops easing pain even though the next dose is not scheduled for several hours)
- You will usually take a small dose of a short acting drug in between other doses usually of a longer acting drug.
- Non-Drug Methods to Manage Pain
Heat:
- Decreases pain, swelling, joint stiffness
- Increases healing
- Includes: baths, hot water bottles, warm moist towels
- Use caution with heat:
- Baths should not be not over 101 degrees
- Heating pads should be on low with cover on the pad to avoid burning the skin;
- do NOT lie on the heating pad
- Do NOT use heat on skin that has recently had radiation
Cold:
- Decreases swelling
- Includes: crushed ice, cold packs, cold wet cloths, gel packs
- Use cold with caution:
- Never put ice directly on skin; place ice bag in towel, pillowcase
- Leave on for no more than 15 minutes at a time
- Do not use on skin that has recently had radiation
Relaxation/Imagery:
- Includes a wide range of activities designed to help you relax and decrease stress, pain and anxiety
- Decreases muscle tension, aches, pains and fatigue
- Includes: muscle relaxation, meditation, visualization, and deep breathing
- Relaxation is considered to be very safe with no to very few side effects
Traditional Healing:
- Talking and working with a Traditional Indian healer
- Spiritual ceremonies to help you and your family with your cancer pain
- Praying together to help relieve your pain
- Addressing spiritual, mental, emotional pains (not just physical)
- Preparing traditional teas, juices, poultices to help relieve your pain
Massage/Pressure:
- Involves the rubbing and kneading of the bodys muscle and soft tissue
- Massage can be shallow and light or firm and deep
- Oils may be used on the skin to prevent irritation
- Massage may decrease stress, anxiety, depression and pain
Acupuncture:
- Involves the use of very fine (thin) needles placed into the body over strategic points to alter body function (such as the feeling of pain)
- Based on ancient Chinese practice that is well accepted by both western providers and traditional Indian healers
- Most people dont feel uncomfortable when the needles are placed
- A licensed acupuncturist should be used
Movement:
- Moving to another position will sometimes lessen the pain
- Sometimes just getting up, walking or other types of movement will leesen the pain
Hypnosis (a form of relaxation):
- A trained hypnotherapist guides the patient into a state of hypnosis with a soothing voice and calming images
- While under hypnosis goals such as being able to control ones pain are suggested
- Helps to train the brain to not recognize the pain or to interpret it as something less uncomfortable
Herbal remedies (teas, herbs):
- Traditional herbs and teas may be helpful in decreasing pain
- Be sure to tell your provider if you are using any traditional teas or herbs
Prayer:
- Suggestion that praying or being prayed for can speed recovery and help with healing
- Prayer may be silent or spoken out loud and can be done alone, in a small group (family) or with a larger group (community, tribe)
Creative Arts:
- Includes such activities as drawing, painting, writing poetry, making music
- These activities can help you express how you are feeling
- May decrease pain by lessening stress and anxiety and providing distraction from the pain feelings
Lifestyle changes:
- Do not do activities that cause pain
- Learn good body mechanics how to move, sit, lift
- Increase rest/relaxation prior to activities
- As possible, do muscle strengthening exercises so as not to strain muscles
- Take pain medicines as ordered
- Let others help you
Other methods/procedures to manage pain
- Cancer treatment
- Radiation or chemotherapy to decrease size of cancer and remove cause of pain
- Nerve blocks
- A specially trained doctor will use a needle to place medicine near a nerve to prevent the sensation of pain
Stopping your pain medicine
- Always talk with your provider before you stop taking your pain medicine
- Never stop your pain medicine suddenly
- Always decrease your pain medicines very gradually (your provider should tell you how to do this)
- If you stop your pain medicines slowly, withdrawal symptoms will not be felt or will be very mild (should you have symptoms, tell your provider immediately)
Important points
- Back pain can be a symptom of the cancer pressing on your spinal cord be sure to tell your provider
- Pain medicines need to be kept out of the reach of children
- Never share your pain medicines with others
- Take your pain medicines as ordered
- Why it is important to Measure Your Pain
You need to use a system that will help your provider know how you feel about your pain and how it affects you
- Tells your provider what your pain is like (sharp, feels like pins and needles)
- Lets the provider know how often it occurs during the day and if any activity caused it (like cleaning salmon which is very hard work
- Helps your provider know what you think is an okay level of pain relief (although my arm and chest area are throbbing, I can work through it)
- Lets your provider know how well the pain relief measures you are using are working (I feel better within fifteen minutes of taking the medication)
Ways to measure your pain
- Keep a pain journal (can be part of a journal of other symptoms)
- Use a pain rating scale numbers, words, pictures
- Use the same method/scale to rate your pain so you can tell your provider how the pain is over time
Pain journals
- Daily pain summary
- Pain level today
- Limit to activities
- Amount of medicine taken
- Pain relief
- Use of non-drug therapies
- Side effects
- Overall satisfaction with pain relief
Pain intensity rating scales
- This helps your provider understand how pain impacts your daily life and your ability to do your daily activities.
- It also helps your provider evaluate the different treatments you are using.
- They may ask you to rate your pain in several ways.
- In many places (hospitals, clinics, or doctors offices) they may ask you to rate your pain on a scale of 0 10.
- What this means is to think about the pain /discomfort/hurt you are experiencing and pick a number that best describes it:
- The numbers from 1-3 may mean that pain is mild but it is not interfering with your ability to do your daily activities,
- The numbers from 4-6 mean that the pain/discomfort/hurt is more noticeable and that it does affect your ability to do your daily activities and you have changed your daily routine because of this,
- The numbers 7-10 means you are having a lot of pain that causes you not to be able to do most of your daily activity and is very intense.
Types of pain intensity rating scales
It takes a while to learn how to use a pain scale. It might be best to try a few different ones to see which is easiest for you to use. The one you choose also should be the best for letting your provider know how much pain you are having.
- Category Scale
None (0) Mild (1-4)
Mild (1-4)  Moderate (5-6)
Moderate (5-6)  Severe (7-10)
Severe (7-10)
- Pain Faces Scales
| 0 No hurt |
2 Hurts just a little bit |
4 Hurts a little bit more |
6 Hurts even more |
8 Hurts a whole lot |
10 Hurts as much as you can imagine |

Numerical Rating Scale
Verbal Descriptor Scale

This scale relies on you using words like those in the arrow above
| Brief Pain Inventory |
 |
Shade areas of worst pain Put an X on area that hurts most |
Causes and Types of Cancer Pain
Causes of Cancer Pain
- Not everyone who has cancer has pain
- For those who do have pain, there are many different causes:
- The cancer itself causes about 65%-80% of cancer pain
- Pressure of the tumor on an organ (liver, lungs), bone or nerves
- Cancer growth into bone, nerves or an organ
- The cancer treatments cause about 15%-25% of pain
- Chemotherapy
- Mouth sores
- Numb fingers, feet
- Bone or joint pain
- Surgery
- Cutting across a nerve during surgery
- Pain from incision
- Radiation therapy
- Nerve ending sensitivity
- Skin irritation
- Procedures for treatment, evaluation or diagnosis (cause about 5%-10% of pain)
- Biopsy (cutting out the cancer or a a piece of the cancer to make a diagnosis)
- Blood draws (using a needle to remove blood from a vein)
- Placing a needle into the spine area (back bone) to give medication (called a lumbar puncture) also could be used to give pain medication
- Not related to cancer or cancer treatment
- Other diseases (diabetes, heart problems, arthritis)
- Injury (car accidents)
The different causes for pain in people with cancer.
- Physical from the cancer or the treatment
- Intellectual - knowledge, memory loss, self-control, review of life issues
- Emotional pain anxiety, fear, grief
- Interpersonal pain burden, physical needs, overprotection
- Financial pain costs, loss of job
- Spiritual pain facing death, questions of faith, feelings
- Bureaucratic pain - more doctors, tests, questions
Types of physical pain:
-
- Acute Pain
- Related to a specific event (surgery, injury)
- Short lasting, as recover from the surgery, the pain at the incision goes away
- Your need for pain medicine is short. You rapidly go from taking strong medicine (a narcotic) to less strong medicine (Tylenol® or Advil®) to no need for pain medicine
- Acute Pain
-
Chronic Pain
- Can last months to years even if cause of pain has healed (surgery) or been removed (chemo done)
- If untreated, pain signals continue and becomes remembered (feelings of pain continue) in your brain even after the pain is gone.
- This is real pain and is not just in your mind.
- Affects your sense of well-being and quality of life.
- Requires the use of pain medicine(s) for longer periods of time, possibly the rest of your life.
-
Phantom (Limb) Pain
- Feeling that the limb or breast is still there even after it has been removed
- May ache, throb or otherwise give you an unpleasant or hurting feeling
- The pain is real even though providers do not know why it happens
-
Neuropathic Pain (involves nerve endings): Nerve damage by tumor or cancer treatment
- The nerve is injured or squeezed by the cancer or cancer treatment.
- Pain may be felt as burning, shooting, stabbing, or numbness. Some say it feels like pins and needles.
- Sometimes called peripheral neuropathy.
-
Breakthrough Pain
- Unexpected pain that occurs between doses of pain medicine (called a pain flare).
- Pain gets very bad in 3-5 minutes
- Pain flares may last about 30 minutes
- Pain flares are not always the same each time you have one
- Usually treated with a pain medicine that acts very quickly and doesnt last for long
- Usually means pain medicine needs to be adjusted (may need more medicine)
- Pain Flares can be caused by:
- Doing something like moving, gardening
- Pain medicine does not last as long or relieve your pain as it should (You have pain before your next dose of pain medicine is due).
- Sometimes there is no obvious cause; the pain flare just happens